Do you have pain on the inside of your ankle? It could be a posterior tibial tendon problem.
As a local physical therapist, I often get questions while coaching or at the local food store or the gym. After I saw a friend wearing a walking boot due to his being recently diagnosed with a suspected posterior tibial tendon injury on a recent trip to the gym, I was inspired to talk about this condition in more detail. He had pain on the inside of his ankle and lower leg and later was told he had an injury to the tendon that runs around the inside of the ankle and foot.
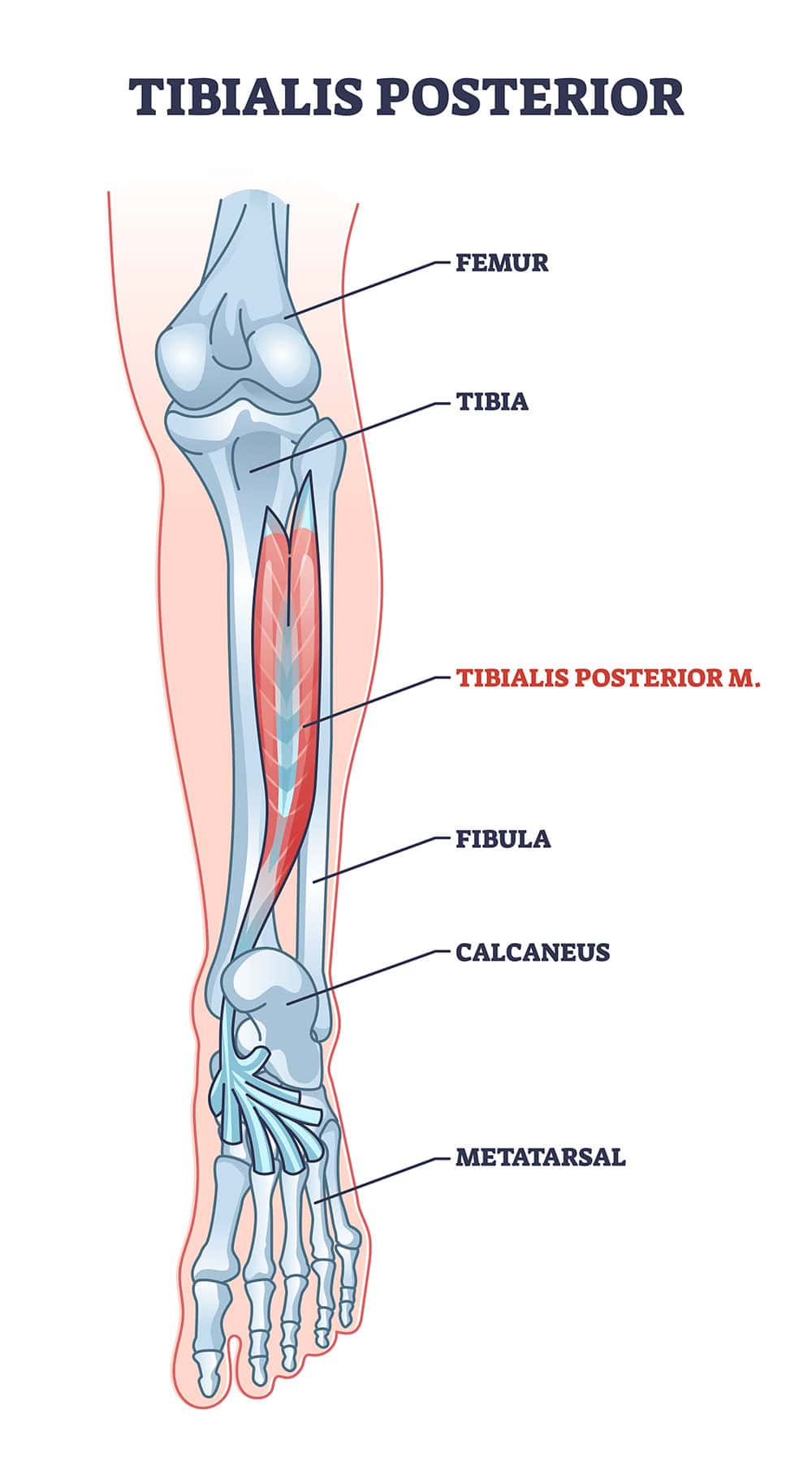
To better understand this condition we first must go over the anatomy and function of this critical structure and its contribution to us walking around this earth comfortably.
We will be looking at a condition termed Posterior Tendinopathy which is an umbrella term for posterior tibial tendonitis “an acute injury” or posterior tibial tendinosis “chronic condition”. To better understand this injury to this tendon let’s first discuss the anatomy and function.
Anatomy and Function of the Posterior Tibial Muscle and Tendon
The tibial posterior muscle is located in the rear compartment of the lower leg. Its upper attachment points in the upper tibia and fibula in addition to the interosseous membrane. As it extends down the inside of the lower leg it becomes tendon and eventually connects to the bottom of the foot in various locations. When the posterior tibial tendon passes just behind the medial malleolus which is the bone sticking out on the inside of the ankle where the tendon is, it makes a turn around this bone to its attachments to various bones in the foot.

It contributes to the movement of the foot to plantar flexion (point the foot down) and inversion (turning the foot inward) when not in contact with the ground. When the foot is in contact with the ground while standing, walking or running it dynamically supports the medial arch of the foot.
Differential Diagnosis – What else can mimic Posterior Tendinopathy
In understanding any problem we first have to arrive at the correct diagnosis prior to treatment. I recommend anyone who is dealing with any orthopedic conditions to get a formal evaluation to avoid wasting time with ineffective treatments or reliance on medications which mask the pain.
A few things can mimic a Posterior Tibial Tendinopathy (PTT). Some common conditions that may be the source of problems which have to be considered before you receive the diagnosis for posterior tibial tendinopathy include:
Flexor Hallucis Longus (FHL) Tendinitis:
Inflammation of the flexor hallucis longus tendon, which runs along the back of the ankle, can cause pain and swelling similar to posterior tibial tendonitis. This condition often occurs due to overuse or biomechanical issues.
Achilles Tendinitis:
Inflammation of the Achilles tendon, which connects the calf muscles to the heel bone, can cause pain and stiffness in the back of the ankle. Achilles tendinitis may present with symptoms similar to posterior tibial tendonitis, especially if the pain radiates to the inner ankle area.
Sinus Tarsi Syndrome:
This condition involves pain and tenderness in the sinus tarsi, a small opening between the talus bone in the center of the ankle and calcaneus or heel bones on the outside of the foot. Sinus tarsi syndrome can cause pain with weight-bearing activities and may mimic the symptoms of posterior tibial tendon problem.
Medial Ankle Sprain:
An injury to the ligaments on the inner side of the ankle can cause pain and instability, which may be mistaken for posterior tibial tendonitis. Medial ankle sprains often occur due to sudden twisting or rolling of the foot.
Tarsal Tunnel Syndrome:
Compression of the tibial nerve as it passes through the tarsal tunnel behind the inner ankle can cause pain, numbness, and tingling in the foot. Tarsal tunnel syndrome may present with symptoms similar to posterior tibial tendonitis, especially if there is associated swelling and inflammation.
Arthritis of the Ankle:
Osteoarthritis or inflammatory arthritis affecting the ankle joint can cause pain, stiffness, and swelling in the ankle region. Arthritis may present with symptoms similar to posterior tibial tendonitis, especially if there is pain with movement or weight-bearing.
Stress Fracture of the Ankle:
A small crack or fracture in one of the bones of the ankle joint can cause pain, swelling, and tenderness. Stress fractures may mimic the symptoms of posterior tibial tendonitis, especially if there is localized pain with activity.
Peripheral Neuropathy:
Nerve damage or dysfunction affecting the peripheral nerves in the lower extremities can cause symptoms such as pain, numbness, and tingling. Peripheral neuropathy may present with symptoms similar to posterior tibial tendonitis, especially if there is pain radiating into the foot.
It's important for your physical therapist to perform a thorough examination, including a medical history and physical assessment. In some cases you may even need diagnostic imaging (such as X-rays, ultrasound, or MRI), to accurately diagnose posterior tibial tendon issue and differentiate it from other conditions with similar symptoms.
What do you experience if you have a Posterior Tibial Tendinopathy (PTT)
Prior to developing posterior tibial tendinopathy patients often have an acute trauma such as a fall, or take part in sports requiring high intensity impact like sprinters to sports like tennis, basketball or soccer with lateral movements. It can even occur from extensive periods of standing or walking more often in older individuals. In the early stages, most younger athletes will have a series of bouts of pain that can resolve with rest, taking an anti-inflammatory, use of orthotics, stretching and strengthening.
As we age, having multiple episodes can eventually lead to a degeneration of the tendon with a loss of blood supply, making the tendon less pliable and less resilient when taking on loads. This can eventually lead to tears. This is often referred to posterior tendinosis with “degenerative tendon” changes versus posterior tendonitis in which “inflammation” is the source of pain and dysfunction. These two conditions can require different treatment approaches.
Most commonly, pain or stiffness with this condition is experienced in the inside of the foot (medial arch), or further up to where the tendon passes close behind the bone on the inside of the ankle (called the medial malleolus). These areas are often tender to the touch, especially after activity. Depending on the severity you may see swelling in these regions. Often the symptoms start after a fall or impact on the lower leg or a repetitive activity.
Certain factors can contribute to you developing these conditions over time.
Everyone has a unique set of factors that lead to this condition. The running and jogging athlete can be quite stubborn about the need for rest especially with a looming race or simply because it serves as such a stress reliever in their life. With this in mind we make every attempt to decrease mileage, duration, intensity or surface type (street versus track), reducing number of days per week or water jogging.
How many people get Posterior Tibial Tendinopathy?
It ranges from 3.3 to 10% of the general population, and is more common among those with diabetes, hypertension, obesity, prior surgery or trauma to the tendon or region, and history of steroid use. In addition, other people at increased risk are those who have been diagnosed with a group of autoimmune disorders: ankylosing spondylitis, psoriatic arthritis, inflammatory bowel disease, reactive arthritis and undifferentiated (J Family Med Prim Care. 2015 Jan-Mar; 4(1): 26–29).
How do we assess if we have a Posterior Tibial Tendinopathy in the clinic?
Diagnosing posterior tibial tendon problems without an MRI typically involves a combination of clinical evaluation and diagnostic tests. Here's how it can be done in bullet points:
Medical History and Physical Examination:
Functional Assessment:
Palpation:
Range of Motion Testing:
Stress Tests:
Diagnostic Imaging (if available and deemed necessary):
It's important to note that while an MRI provides detailed information about the status of the posterior tibial tendon and surrounding structures, a clinical diagnosis can often be made based on a thorough history, physical examination, and ancillary tests when available.
How do we treat this condition
Understand the history of the problem
First thing is to understand the patient’s history of the problem.
Orthotic or Changes in Footwear
Once we determine a strategy to reduce stress through modified rest, we often look at ways of cross training to prevent deconditioning in our patients. This can range from aquatic training to rowing or a stationary bike. We make every attempt to not completely shut down cardiovascular training in order to maintain a patient's endurance.
One way of helping aid in the recovery is to use an over the counter soft insert for all shoes you are wearing and donning shoes whenever you are in the house. In the early stages using a custom hard insert can be irritating to the patient. Even if you are currently using a custom hard orthotic it can be helpful to temporarily use a soft insert until the condition improves.
Stretching the foot and ankle complex
This can be helpful or it can aggravate a patient’s condition. We have this natural desire to stretch anything that hurts, but this is not always the solution and, in some cases, it delays your progress. I give the analogy that you wouldn’t want to bend a cut on your knuckle if it has recently been stitched. In the early stages of a true posterior tibial tendonitis, stretching an inflamed tendon can irritate the tissues trying to heal and prolong the recovery. If it has been going on for longer than 6-8 weeks, then it is generally a reasonably safe time to start.
When we do stretch a combination the following stretches can be helpful:
All stretches can be initially held for 1-2 seconds and for 10-15 repetitions. Eventually you'll progress to 6 repetitions for a minimum of 30 seconds each. We start with short duration stretches to minimize irritation in the early stages of recovery. Each stretch should feel like you are experiencing firm pressure and any discomfort should resolve within a minute or two after your stop stretching.
Strengthening Exercises for Posterior Tibial Tendinitis or Tendinosis
In the early stages direct strengthening of the foot and ankle complex can further aggravate the healing tendon. To decrease the chance of deconditioning and assist in recovery we look at strengthening about and below the injured structure. In cases of a posterior tibial tendon injury we will focus on strengthening and stretching at the knee, hip and trunk on both sides. We focus on the early stages of healing with strengthening of the following:
In 1- 2 weeks depending on the stage of healing we can introduce direct strengthening of the foot and ankle complex using isometric strengthening then progressing to isotonic strengthening.
Let’s discuss the differences between isometric strengthening and isotonic strengthening.
Isometric Strengthening:
Isometric strengthening is a type of muscle strengthening exercise where the muscle contracts and generates tension without changing its length. During isometric exercises, the joint angle and muscle length remain constant. For example, holding a plank position engages the core muscles isometrically. Isometric exercises are beneficial for improving muscle endurance and stabilizing joints. They can be particularly useful in rehabilitation settings to strengthen muscles without placing excessive stress on injured tissues.
Isotonic Strengthening:
Isotonic strengthening involves muscle contractions where the muscle changes length while resisting a constant load. In isotonic exercises, the muscle contracts to move a joint through a range of motion, causing the muscle length to change. For example, performing bicep curls with dumbbells involves isotonic contractions of the bicep muscles as they contract to lift the weight. Isotonic exercises are effective for building muscle strength, endurance, and promoting muscle growth. They are commonly used in resistance training programs to target specific muscle groups and improve overall fitness levels.
In the early stages we typically start with isometric strengthening which in certain cases can reduce or eliminate tendon related pain in addition to providing gentle strengthening. In both my experience and according to the research, isometric exercises can occasionally irritate the tendon and you may need to switch to gentle isotonic exercises that are much better tolerated. When working with patients I will start with gentle isometrics progressing the intensity from mild to moderate pressure and increase the time from 10 second to 45 seconds as described by Jill Cook on her research on Achilles’ tendon problems.
In most cases complete rest is not optimal. It is pretty well accepted that completely resting a tendon can delay healing and delay the return of the patient to full health and unrestricted activity.
Good luck!


